New Anthrax Vax May Prove More Palatable
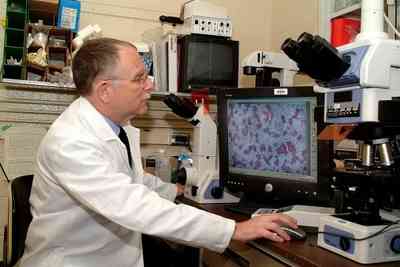
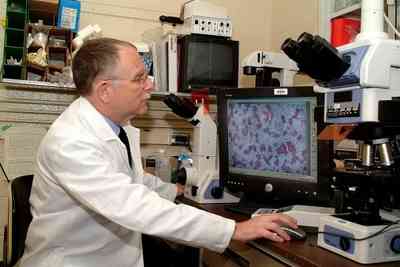
The next-generation anthrax vaccine, based on a decade of work
at the U.S. Army Medical Research Institute of Infectious Diseases,
is now moving into not one, but four clinical trials.
The group at the institute did the legwork for the current
vaccine candidates by singling out which protein in Bacillus
anthracis -- the bacterium that causes anthrax -- signals the
body to produce immunity to the disease.
Early studies established definitively that the protein called
"protective antigen" was just the component the vaccine would
require, said Dr. Arthur Friedlander, a senior scientist at
USAMRIID who directed the group's long-term effort. After
discovering the protein, researchers took the gene that codes for
protective antigen and used recombinant DNA technology to try to
produce the protective antigen in three expression systems:
bacteria, yeast and viruses.
Ultimately, the team found bacteria was the best for producing
the protein, and decided to grow the protective antigen in a
non-disease causing strain of B. anthracis. The resulting
recombinant protective antigen, or rPA, should provide a high
degree of safety in a vaccine because it's just one building block,
a single protein of the organism that can produce an immune
response.
Researchers then proved it was effective in the best animal
model available, the non-human primate. "What we did was identify
it, purify it to a very high degree and showed that this protein by
itself was protective in the most relevant animal model of human
inhalational anthrax,"
Friedlander said.
Research Locations Pinpointed by Army (More TFRs Coming?)
To date, two clinical trials that use the B.
anthracis-based rPA are underway. VaxGen, based in Brisbane
(CA), started its clinical trials at Baylor College of Medicine,
Texas; Emory University School of Medicine in Atlanta; Johns
Hopkins University in Baltimore and Saint Louis University Health
Sciences Center. The test is under a contract from the National
Institute of Allergy and
Infectious Diseases.
In a collegial effort, the National Institute of Allergy and
Infectious Diseases, USAMRIID and the Joint Vaccine Acquisition
Program have undertaken a Phase I clinical trial at the University
of Maryland using a version of the original USAMRIID formulation
manufactured at the National Cancer Institute Frederick (MD).
The University of Maryland trial will help advance the
development of the other vaccines, said Dr. Lydia Falk, director of
the Office of Regulatory Affairs, in the Division of Microbiology
and Infectious Diseases at the National Institute of Allergy and
Infectious Diseases.
"We can begin to compare the responses we see in humans to what
had been observed in animals," she said. "That's a critical part of
the development of these vaccines. The more preliminary
investigative work that we can do, the more it benefits the entire
field. Our hope is that the information we gain will be able to add
to those building blocks that would lead to an accelerated
development plan."
FDA Won't be a Roadblock
 The formulation being used in that
trial won't be pushed toward Food and Drug Administration
licensing. "The product that is available and the one that was used
during USAMRIID's preclinical studies had the rPA protein in one
tube and an aluminum adjuvant in another tube, and before you
injected it, you mixed the two," Falk said. "That's not an easy
formulation to take to licensure." However this trial design will
determine the value of including an adjuvant in the final vaccine
formulation.
The formulation being used in that
trial won't be pushed toward Food and Drug Administration
licensing. "The product that is available and the one that was used
during USAMRIID's preclinical studies had the rPA protein in one
tube and an aluminum adjuvant in another tube, and before you
injected it, you mixed the two," Falk said. "That's not an easy
formulation to take to licensure." However this trial design will
determine the value of including an adjuvant in the final vaccine
formulation.
Two companies are currently using rPA grown in E.
coli to create their next generation anthrax vaccine
candidates. An rPA vaccine from the UK-based Avecia, under a
contract with the National Institute of Allergy and Infectious
Disease, will soon start Phase I clinical trials.
The second company, Dynport Vaccine Company, LLC, which licensed
its rPA product from Avant, began its Phase I clinical trial April
28. The trial is being conducted by the Henry M. Jackson Foundation
in Rockville (MD), which routinely pursues vaccines for HIV for the
military.
Because the foundation had an HIV vaccine candidate that used
rPA as one of its two components "we decided to reprioritize our
activities and commit to evaluating this protective antigen after
the anthrax mail attacks in October 2001," said Dr. Merlin Robb of
the Henry M. Jackson Foundation, the principal investigator for the
foundation's clinical trial. "(The rPA) was ready to go into humans
to evaluate it for an anthrax indication. We sensed that it was a
higher national priority."
Although the rPA vaccines are on an advanced development path
toward Food and Drug Administration licensure, USAMRIID scientists
still lend their expertise to vaccine manufacturers and the
National Institute of Allergy and Infectious Diseases.
"Their contributions can't be overstated," said Dr. Ed Nuzum,
the project officer providing technical oversight for the two
National Institute of Allergy and Infectious Diseases contracts
with Avecia and VaxGen. "Because of the work done at USAMRIID, as
well as its counterpart in the United Kingdom, the Defence Science
and Technology Laboratories, the rPA-based vaccine candidates are
the most advanced second generation anthrax vaccines."
USAMRIID's early development work regarding animal
studies and assay development will also be critical for developing
animal models for Food and Drug Administration approval under the
"Animal Rule." The rule, effective in July 2002, permits use of
data from animal studies when efficacy studies of new drugs or
biological products against chemical, biological, radiological or
nuclear substances in humans is impossible because of the rarity of
the disease or because human exposure to potentially lethal agents,
like anthrax, is unethical.
"This is the first test case of the concept of licensing a
vaccine based on animal efficacy data and trying to correlate that
with the human immune response," Friedlander said.
Nuzum said he thinks the rPA vaccines are potentially the best
vaccines to be going forward for licensure under the animal rule
largely because of the work done at USAMRIID and DSTL. "The data,
models and assays really are essential to the foundation for the
work we're doing now," he said.
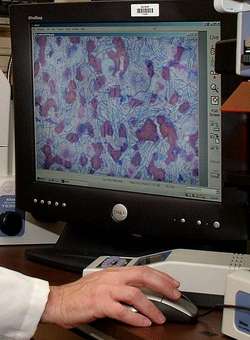
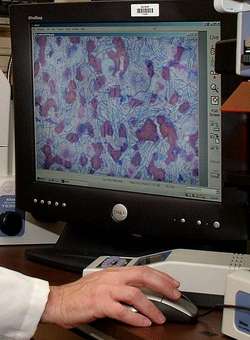
[Thanks to Karen Fleming-Michael, reporter at Fort Detrick (MD),
and the American Forces Press Service. Photo by Larry
Ostby --ed.]
 ANN's Daily Aero-Linx (12.12.25)
ANN's Daily Aero-Linx (12.12.25) ANN's Daily Aero-Term (12.12.25): Land And Hold Short Operations
ANN's Daily Aero-Term (12.12.25): Land And Hold Short Operations ANN FAQ: How Do I Become A News Spy?
ANN FAQ: How Do I Become A News Spy? NTSB Final Report: Cirrus Design Corp SF50
NTSB Final Report: Cirrus Design Corp SF50 Airborne 12.08.25: Samaritans Purse Hijack, FAA Med Relief, China Rocket Fail
Airborne 12.08.25: Samaritans Purse Hijack, FAA Med Relief, China Rocket Fail